Infertility Male and Female
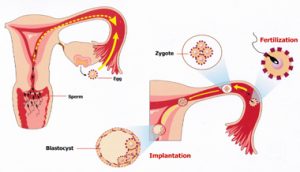
Inability of a couple to conceive after 1 year of regular unprotected intercourse can be termed as infertility.
When the age of the female partner is more than 35, infertility treatment can be started after 6 months of regular unprotected intercourse.
Causes of Infertility
Female Factor
- Ovulatory dysfunction
- Tubal dysfunction
- Endometriosis
- Uterine factors
- Diminished ovarian reserve
Other Causes: Cervical factor, immunological infertility, etc.
Male Factor
- Oligospermia
- Azoospermia
Combined Factors
- Unexplained infertility
We individualize the infertility treatment for each and every couple. At Shalby infertility clinic, all infertility patients receive pre-conceptional care before commencing actual treatment. For optimizing the treatment; medical, lifestyle, emotional & nutritional factors should be an integral part of fertility therapies.
Approach to Female infertility
Management of the patients can only be appropriately provided once the cause/s of the problem are discovered, which in turn requires detailed history, physical examination and appropriate investigations to be undertaken.
Traditionally, infertility investigations are generally started after a year of involuntary infertility. However, it can be started earlier in some cases like advanced female age, chronic anovulation or a history of previous pelvic surgery.
Pelvic Ultrasound
-
- It gives accurate noninvasive assessment of the pelvic organs.
- Baseline Ultrasound scan is used for congenital anomalies, uterine fibroids, hydrosalpinges, ovarian cysts, endometriomas, polycystic ovaries, and ovarian volume with antral follicle count.
- Saline Sonography may be used to differentiate thick endometrium from submucus fibroid and endometrial polyp. It can also be used to differentiate thin endometrium from Ashermann’s syndrome.
- Color & pulsed Doppler ultrasound can be used to predict ovarian responsiveness to gonadotropin stimulation and endometrial receptivity to embryo implantation.
- 3D technology may be used to diagnose different uterine abnormalities and assessing its degree of interference with endometrial cavity. Ovarian volumes and endometrial volumes can be measured accurately with 3D technology which helps in prediction of success of an IVF cycle.
Tests for ovulation
-
- BBT (Basal body Temperature) charts: generally not advocated as it is cumbersome for the patient
- Serial ovarian ultrasound for follicular study: preferred method
- Mid luteal serum progesterone level
- Assessing LH surge by measuring blood/urine LH level
- Endometrial biopsy: not routinely preferred as it do have wide variation in results
- Tests for tubal function
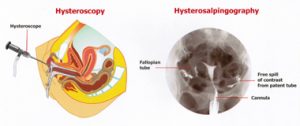
- HSG (most widely used tubal patency test): It has added advantage of diagnosing uterine defects like fibroids, polyps & synechia. It has got disadvantage of limited ability to assess peritubal adhesions and infection risk. HSG has 65% sensitivity & 83% specificity in diagnosing tubal obstruction.
- HyCoSy (Hysterosalpingo Contrast Sonography): Tubal patency is assessed using transvaginal ultrasound and an injection of a solution containing gas microtubules stabilized on Galactose microparticles. It has got the advantage of avoidance of X-ray exposure and assessment of ovaries simultaneously.
- Salpingoscopy & Falloposcopy: It is possible to examine whole length of fallopian tube using these methods. Currently, both approaches are of research interest only.
- Laparoscopy: It is gold standard test for assessing tubal patency.
Approach to Male Infertility
- Abnormalities in sperm production or function can account for 35 -40% of all cases of infertility.
- Semen Analysis: It is the hallmark of male infertility evaluation.
- Specimen is to be obtained following 2-7 days of abstinence from sexual activity, preferably obtained with masturbation in sterile, plastic, wide mouth container. Semen should be delivered to the laboratory within 30 minutes of collection and to be transported at room temperature.
World Health Organization (WHO) semen analysis parameter normal values:
- Liquefaction Complete within 60 minutes at room temperature
- Appearance Homogenous, gray & opalascent
- Consistency leaves a pipette as discrete droplets
- Volume 2 ml or more
- pH 7.2 or more
- Concentration 20 million sperms/ml semen or more
- Total number 40 million sperms per ejaculate or more
- Motility 50% or more with forward progression, or 25% or more with rapid progression within 60 minutes of collection
- Morphology 30% or more with normal forms
- Vitality 50% or more
- Leucocytes Fewer than 1 million/ml
In azoospermic or oligospermic men, Serum FSH level and Scrotal Sonography with Doppler can be helpful.
Contact Shalby Hospital for Infertility Treatment in India.
Shalby Hospital
Infertility and IVF
Center Of Excellence
- Arthroscopy – Sports Injury
- Ophthalmology and Glaucoma
- Oncosurgery
- Oncology
- Obstetrics and Gynaecology
- Obesity Surgery
- Neuro Science
- Neurosurgery
- Nephrology
- Orthopedic and Trauma
- Paediatric Orthopedics
- Spine Surgery
- Rheumatology
- Radiology and Imaging
- Pulmonology and Chest
- Plastic Surgery
- Paediatrics and Neonatology
- Pathology And Microbiology
- Maxillofacial Surgery
- Knee Joint Replacement
- ENT Surgery
- Endoscopy and Laparoscopy
- Endocrinology – Diabetology
- Emergency Medicine
- Dental Cosmetic and Implantology
- Cosmetic and Aesthetic
- Cardiothoracic and Vascular Surgery
- Cardiology
- Gastrointestinal Surgery
- Gastroenterology
- Intensive and Critical Care
- Infertility and IVF
- Infectious Diseases
- Hip Joint Replacement
- Liver Transplant
- Hair Transplant
- General Surgery
- General Medicine
- Uro Surgery
- Dermatology
- Arthroplasty
- Psychiatry
- Urology
- Anesthesia












